Coronavirus may be aided by body's own immune response to enter more cells: Study
One of the human body's main defences against viral infections may be helping the novel coronavirus infect more cells, according to a study which can help understand why some people are more susceptible than others to COVID-19.
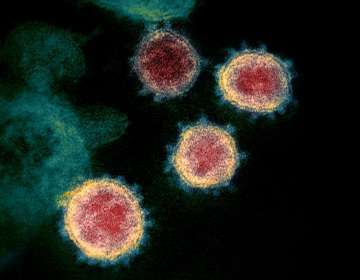
One of the human body's main defences against viral infections may be helping the novel coronavirus infect more cells, according to a study which can help understand why some people are more susceptible than others to COVID-19. The study, published in the journal Cell, used single-cell RNA sequencing, which identifies which of roughly 20,000 genes are "on" in individual cells, and found that only a tiny percentage of human respiratory and intestinal cells make the proteins that help the virus gain entry into human cells.
"We started to look at cells from tissues such as the lining of the nasal cavity, the lungs, and gut, based on reported symptoms and where the virus has been detected," said Jose Ordovas-Montanes, study co-author from Boston Children's Hospital in the US. "We wanted to provide the best information possible across our entire spectrum of research models," Ordovas-Montanes said.
Recent studies had pointed out that the novel coronavirus, SARS-CoV-2, like the closely related SARS-CoV behind the 2002-03 SARS pandemic, uses a receptor called ACE2 to gain entry into human cells, aided by an enzyme called TMPRSS2. In the current research, the scientists found that only a small fraction of cells, often well below 10 percent, make both ACE2 and TMPRSS2.
They said these cells fall in three categories -- goblet cells in the nose that secrete mucus, lung cells known as type II pneumocytes which help maintain the alveoli sacs where oxygen is taken in, and one type of so-called enterocytes that line the small intestine and aid in nutrient absorption. "Many existing respiratory cell lines may not contain the full mix of cell types, and may miss the types that are relevant," Ordovas-Montanes said.
"Once you understand which cells are infected, you can start to ask, 'How do these cells work?' 'Is there anything within these cells that is critical for the virus's life cycle," he explained. With further studies, the researchers said they can perform better screens to find what existing drugs target the biological mechanism of COVID-19. Ordovas-Montanes and his team also found that the ACE2 gene, which encodes the receptor used by SARS-CoV-2 to enter human cells, is stimulated by interferon -- one of the body's main defenses when it detects a virus.
They said this signalling molecule used by cells to communicate with each other about infection, turned the ACE2 gene 'on' at higher levels, potentially giving the virus new portals to get in. "ACE2 is also critical in protecting people during various types of lung injury," Ordovas-Montanes said. "When ACE2 comes up, that's usually a productive response. But since the virus uses ACE2 as a target, we speculate that it might be exploiting that normal protective response," he added.
And since interferon also plays a major role in the body's own natural immune response against viruses, the scientists believe the timing of when the molecule is active in the body compared to the virus infection process is key to its effects. "It might be that in some patients, because of the timing or the dose, interferon can contain the virus, while in others, interferon promotes more infection," said Ordovas-Montanes.
"We want to better understand where the balance lies, and how we can maintain a productive antiviral response without producing more target cells for the virus to infect," he added. The scientists also believe that it is too soon to relate the findings to the runaway inflammatory response, called the cytokine storm, reported in very sick COVID-19 patients.
They explained that cytokines are a family of chemicals that rally the body's immune responses to fight infections, adding that interferon is part of this family. "It might be that we're seeing a cytokine storm because of a failure of interferon to restrict the virus to begin with, so the lungs start calling for more help. That's exactly what we're trying to understand right now," Ordovas-Montanes said.